Providing Financial Incentives and Behavioral Nudges to Encourage Covid-19 Vaccine Uptake in the United States
- General
- Health outcomes
- Incentives
- Information
- Preventive health
The large number of people who have remained unvaccinated or partially vaccinated during the Covid-19 pandemic, despite sufficient vaccine supply, has generated interest in incentives and nudges that may encourage vaccine take-up among the vaccine hesitant. In this study, researchers evaluated the impact of financial incentives, public health video messages, and access to a vaccine scheduling link on Covid-19 vaccination intentions and vaccine take-up. Researchers found that after thirty days none of the interventions led to increases in vaccine take-up among those who received them compared to those who did not. Additionally, in exploratory analysis, financial incentives were found to reduce vaccination rates among certain subgroups, highlighting the potential for financial nudges to backfire. In a subsequent study, researchers evaluated the impact of personal reminder messages and financial incentives, on the take-up of Covid-19 booster vaccination rates. After two weeks, personal reminder messages led to increases in booster vaccination rates while monetary incentives had no additional impact.
Policy issue
Despite ample supply of the Covid-19 vaccine in the United States, millions of Americans remain unvaccinated or partially vaccinated. Vaccine hesitancy in the United States is affected by many complex factors including political beliefs, concerns about safety, and mistrust of the medical profession. The large proportion of Americans who have remained unvaccinated during the Covid-19 pandemic has generated interest in how to encourage vaccine and booster take-up and dispel vaccine hesitancy.
To combat Covid-19 vaccine hesitancy, many local governments and employers have offered financial incentives and implemented other behavioral nudges to increase vaccine take-up. Such strategies have been successfully employed to increase vaccinations for other infections such as influenza. However, evidence on the effectiveness of nudges at increasing Covid-19 vaccinations remains limited. Furthermore, most of the current evidence focuses on vaccine intentions rather than vaccine take-up.
Context of the evaluation
Contra Costa County is a racially diverse suburban county in the Bay Area of California. At the time of the study, it had one of the highest countywide vaccination rates in California. Due to receiving increased vaccine supply from the federal government, the county was able to open eligibility for vaccinations to all adults by the end of March 2021, several weeks before the State of California.
Individuals selected for the first study sample were unvaccinated members of the Contra Costa Health Plan (CCHP), the public Medicaid managed care plan in Contra Costa County. As a result, this study focused on individuals who had delayed receiving a vaccine despite weeks of eligibility and sufficient vaccine supply. The average age of an individual in the study sample was 36 years old and 74 percent of the study sample was female, which reflects the higher representation of adult women in the Medicaid program. The median household income was between $20,000 to $29,999.
Individuals selected for the subsequent study were Contra Costa Regional Medical Center (CCRMC) patients who had previously received a full two-dose primary series Covid-19 vaccination and were due for a Covid-19 booster vaccination, but had not scheduled one. Study participants on average had received a first Covid-19 vaccination 1.5 years before the date when the reminder messages were sent. The mean age of an individual in the study sample was 43 years old. Nearly 75 percent of study participants had primary insurance coverage through the state of California’s Medicaid program, Medi-Cal.

Details of the intervention
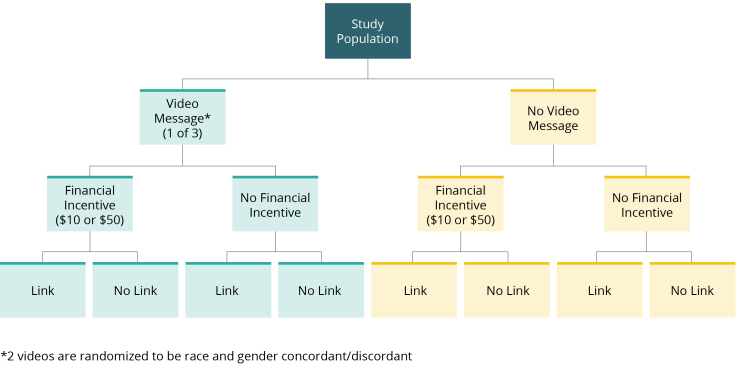
In the initial study, researchers evaluated the impact of public health video messages, financial incentives, and a vaccine scheduling link on Covid-19 vaccination intentions and vaccine take-up.
First, individuals were invited to complete a short internet-based survey. All survey participants were then randomized to watch one of three public health video messages (California Department of Health message, safety message, health consequences message) or no video. The safety message and health consequences message were randomized to be race and gender concordant/discordant between the participant and the physician in the video.
In addition, survey participants were randomly assigned to receive either a financial incentive of $10 or $50 or no financial incentive for getting vaccinated within two weeks of survey completion.
Lastly, participants were also randomly assigned to receive either a link to the county’s public vaccination appointment scheduling system or a message about getting vaccinated without a link.
In the subsequent study, researchers evaluated the impact of personal reminder messages and financial incentives on Covid-19 booster vaccine take-up.
Individuals in the sample were randomly assigned to receive a reminder message, a reminder message with a financial incentive of $25 for getting boosted, or no reminder message or incentive. Study participants were also randomly assigned to receive either email or text message reminders to account for potential differences in response rates and the contact information on hand.
Results and policy lessons
Results from both studies suggest financial incentives do not increase patients’ likelihood to get vaccinated or boosted against Covid-19. While in the initial study, some interventions increased patients’ vaccination intentions, these increases did not translate to increased vaccination take-up. In the subsequent study, reminders increased Covid-19 booster vaccination rates.
Initial study results
After thirty days, none of the interventions in the initial study (video messages, financial incentives, scheduling link) led to increases in vaccine take-up among those who received them compared to those who did not.
In the comparison group, 8.8 percent of participants were vaccinated within thirty days of survey completion. All of the intervention groups experienced small, close to zero treatment effects that did not improve upon the comparison group’s rate. Furthermore, exploratory analysis showed that among older individuals and those who supported Trump in the 2020 presidential election, financial incentives actually reduced vaccination rates, highlighting the potential for financial nudges to backfire. For respondents aged 40 and over, thirty day vaccination rates declined by 4.5 percentage points and 4.7 percentage points in response to the $10 and $50 incentives respectively. For respondents who indicated they supported Trump in the 2020 presidential election, vaccination rates declined by 4.2 percentage points in response to the $50 incentive.
Vaccination intentions increased by 5.5 percentage points in response to the safety video message and 8.6 percentage points in response to the health consequences video message. However, the relationship between vaccination intentions and vaccine take-up was relatively weak, with a 10 percentage point increase in vaccination intention associated with a 1.5 percentage point increase in vaccine take-up. While vaccination intentions may be a useful way to study the impact of different policies and can be illuminating in other contexts (e.g., influenza vaccinations), such studies may have limited value for Covid-19 vaccinations.
Race concordance between physicians in the video messages and study participants was found to not affect vaccination intentions or vaccine take-up. Gender concordance did not have an effect on vaccination intentions but did seem to matter for vaccine take-up. For example, assignment to a gender-discordant physician decreased thirty day vaccination rates for the health consequences video message by 2.9 percentage points.
Based on these results, Contra Costa Health Services de-emphasized financial rewards for Covid-19 vaccinations. This study suggests that strategies that have proved popular in the past, such as financial incentives, are unlikely to yield the high vaccination rates needed to reduce transmission and morbidity of Covid-19. As a result, policymakers and practitioners should set realistic expectations of what nudges are able to accomplish during this pandemic and understand that achieving high vaccination rates will likely require much stronger policy actions.
Booster study results
In the subsequent study, researchers found that reminder messages increased booster vaccination take-up by 0.86 percentage points (32.5 percent increase from a baseline of 2.65 percent). Small financial incentives had no additional impact on vaccination rates compared to reminders without financial incentives. Reminder messages plus financial incentives increased overall vaccination take-up by 0.82 percentage points (31.3 percent increase from a baseline of 2.65 percent).
Effects on subgroups
Reminder messages with and without financial incentives increased booster take-up more for individuals over 65 years old than for younger individuals. Reminders increased take-up by 2.73 percentage points (107.91 percent increase from a baseline of 2.53 percent) for those over 65 years old relative to a 0.49 percentage point increase (19.37 percent increase from a baseline of 2.53 percent) for those under 65. Reminders plus financial incentives increased take-up by 1.73 percentage points (68.38 percent increase from a baseline of 2.53 percent) for those over 65 relative to a 0.63 percentage point increase (24.90 percent increase from a baseline of 2.53 percent) for those under 65.
The interventions were also most effective among groups with low baseline booster vaccination rates, including those messaged by SMS and Spanish speakers.
Reminders via SMS increased take-up by 1.30 percentage points (64.36 percent increase from a baseline of 2.02 percent) while reminders via email increased take-up by 0.59 percentage points (29.21 percent increase from a baseline of 2.02 percent). Reminders via SMS plus incentives increased take-up by 1.32 percentage points (65.35 percent increase from a baseline of 2.02 percent) while reminders via email plus incentives increased take-up by 0.52 percentage points (25.74 percent incrase from a baseline of 2.02 percent). Additionally, Spanish-language reminders increased vaccination booster rates more than English-language reminders. Spanish-language reminders increased take-up by 1.77 percentage points (77.63 percent increase from a baseline of 2.28 percent) while English-language reminders increased take-up by 0.57 percentage points (25.00 percent increase from a baseline of 2.28 percent); Spanish-language reminders plus incentives increased booster take-up by 1.03 percentage points (45.18 percent increase from a baseline of 2.28 percent) while English-language reminders plus incentives increased booster take-up by 0.73 percentage points (32.02 percent increase from a baseline of 2.28 percent).
There were no measurable differences in impacts by gender, race or ethnicity, or insurance type for those who were insured.
These findings indicate that reminder messages can increase Covid-19 booster take-up, especially among groups with low baseline vaccination rates, whereas small financial incentives are unlikely to yield additional increases.

