Messaging Strategies to Promote Safe Water and Hygiene in Bangladesh
- Families and households
- Take-up of program/social service/healthy behavior
- Water quality
- Information
- Water, sanitation, and hygiene
Lack of access to clean water is a major environmental and health challenge in many low- and middle-income countries. Researchers tested whether sharing messages that appealed to negative emotions, like shame or disgust, increased households’ hand washing behavior and willingness to pay for water chlorination in Dhaka, Bangladesh. Negative messaging had no impact on chlorination levels or willingness to pay, but the provision of low-cost hand washing facilities did increase hand washing.
Policy issue
Diarrheal diseases caused by the consumption of contaminated water are among the top causes of death around the world.1 The highest mortality rates are found in South Asia and Sub-Saharan Africa, with Bangladesh reporting 31.16 deaths per 100,000 people in 2019.2 Water-borne diseases also negatively impact human capital development. Proven solutions to the adverse effects of unclean water include safe sanitation, water treatment, and hand washing. However, barriers like lack of information, incorrect beliefs about good health practices, and present bias can preclude individuals from taking up such solutions. Furthermore, the provision of clean water requires large-scale investment, which can be costly and challenging to coordinate from a governance perspective.
Existing evidence shows that interventions seeking to provide information and reduce financial costs have had little success in changing sanitation behaviors and public health outcomes. With that in mind, can messaging that emphasizes negative emotions and social pressure increase hand washing behavior and the use of and willingness to pay for chlorine-based water treatment?
Context of the evaluation
In the informal settlements of Dhaka, Bangladesh, where this evaluation took place, most families live in compounds composed of 4 to 18 households that share a courtyard, toilet, water source, and cooking facilities. The setup allows for easy observation of both water collection and hand washing by members. Most of these compounds have poor quality water and a high incidence of water-borne diseases like cholera and diarrhea.
Organizations such as the implementing partner, International Center for Diarrhoeal Disease Research (icddr,b), have been working with these communities to promote sanitation efforts. Five communities in Dhaka—Mohamedpur, Mirpur, Badda, Khilgaon, and Bashabo—were chosen for this evaluation based on their poor water quality, high levels of water-borne disease, and high population density. Before the intervention, only 22 percent of compounds had access to water and soap for hand washing and only 63 percent reported consistently boiling water before drinking.
Details of the intervention
Researchers partnered with icddr,b to conduct a randomized evaluation to test the impact of messages emphasizing negative emotions and social pressure on hand washing and willingness to pay for chlorine-based water treatment.
Researchers randomized a total of 434 compounds to two different interventions:
- Negative emotions and social pressure message (217 compounds): Compounds in this group received messages highlighting the presence of fecal matter in or on soiled objects and their neighbors’ role in spreading fecal matter as well as urging individuals to observe their neighbors’ behavior.
- Standard health message (217 compounds): Compounds in this group received messages highlighting the risks of untreated water, how water treatment can reduce health risks, and how improving their health also improves the health of others. This served as a comparison group.
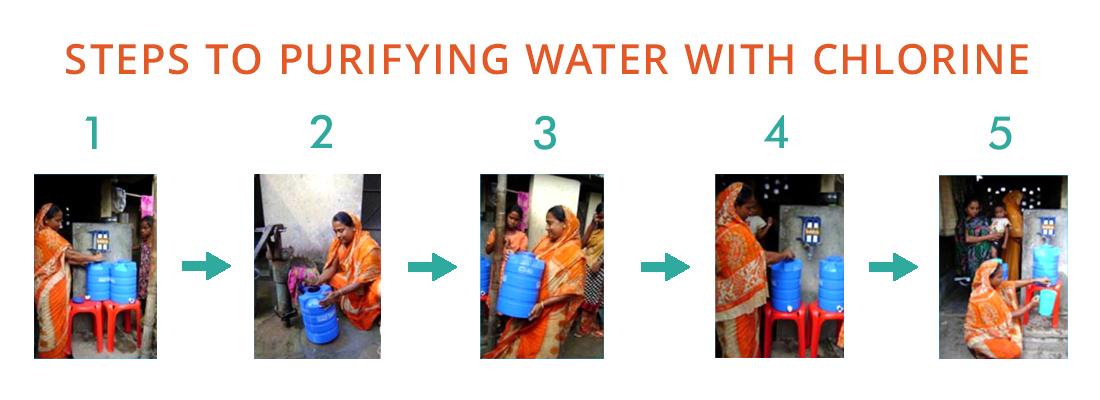
In all participating compounds, the implementing partner conducted one of the two promotional meetings and provided a four-month trial of an easy-to-use chlorine dispenser, two 15-liter reservoirs to save water, and two plastic stools to help dose water.
Two-thirds of the compounds (291 in total) were further randomly assigned to receive a hand washing intervention, which included additional messaging on hand washing as well as a sample of a low-cost “soapy water bottle,” a plastic water bottle to combine packets of mixed powdered soap and tap water, to test the effect of such hardware on the presence of soap and hand washing.
Following the four-month free trial of the chlorine dispenser, researchers measured residents’ willingness to pay (WTP) for a year’s subscription for the dispenser by randomizing compounds into two groups:
- Group auction (217 compounds): Compound residents in this group were asked for their collective WTP.
- “Weakest link” auction (217 compounds): Compound residents in this group were asked for their individual or household WTP and willingness to contribute to public goods for the compound.
Outcome measures of interest were the availability of soap and water near latrines (a proxy for hand washing with soap after defecation), observed hand washing with soap, and free residual chlorine in household drinking water. To determine the impact on demand, researchers measured each compound’s willingness to contribute money to a shared chlorine dispenser. The availability of soap and water was checked at baseline, midline, and endline during the messaging intervention and hand washing was measured during five-hour observation sessions at each compound starting two months after the free trial began.
Results and policy lessons
Negative emotions and social pressure messaging did not lead to higher levels of water chlorination or substantial willingness to pay for water treatment hardware when compared to the standard messaging group. The hand washing treatment, on the other hand, led to increased hand washing and availability of soap and water.
Water Treatment: Two months after health messaging was initially provided, 11.8 percent of households in the negative messaging group had measurable levels of chlorine in their drinking water compared to 8.5 percent of households in the comparison group—a 38.8 percent increase. However, this differential effect of the negative emotions and social pressure message was gone by the free trial’s conclusion, with chlorination rates reaching approximately 8 percent in both message groups.
Availability of Soap and Water: The hand washing intervention increased the availability of soap and water at compound latrines. At the culmination of the free trial, soap and water were found at latrines in 58.5 percent of compounds that received the hand washing intervention compared to 15.9 percent of compounds that did not—a 267.9 percent increase. Researchers found no differences on availability of soap and water based on whether the compounds received the negative emotions and social pressure messaging or the standard health messaging in addition to the hand washing intervention. Finally, the likelihood of the presence of soap and water in compounds that lost the free auction for the dispenser fell from midline to endline by 15.3 percentage points (from 51 percent to 35.7 percent), suggesting some habit formation but also sensitivity to price.
Hand Washing: The hand washing intervention improved hand washing behaviors—two months after the program started, the rate of hand washing with soap after using the toilet was 15 to 17 percent in compounds that received the hand washing intervention compared to 10 to 11 percent in compounds that did not (an increase of 4.8 to 6 percentage points). There was no effect on the use of water with or without soap to wash hands, suggesting the importance of easier access to soap for those who would like to wash their hands in improving behavior, and not an increased likelihood of hand washing among those who otherwise would not. Additionally, researchers found the hand washing intervention to be inexpensive, costing about US$0.75 per household per year. Even though participants reported greater dislike of untreated water, these effects were not sufficient to shift hand washing behavior resulting in no differences in hand washing rates between the negative emotions and social pressure and standard message groups.
Willingness to Pay (WTP): The average WTP was not significantly higher in the negative emotions and social pressure group than in the standard group (US$0.58 compared to US$0.52 per compound per month) and similarly the hand washing intervention had no effect. The average WTP for the chlorine dispenser after the free trial was only US$0.14 per household per month, however this low WTP is not easily explained by an apathy toward water treatment. Later research in comparable households among these same Dhaka communities found that WTP for a ceramic water filter was about US$17. This suggests that the low WTP for the chlorine dispenser relative to the later-tested filter may be due to dislike of the dispenser or chlorine, the challenges of group agreement on collective payment, or other factors like safe storage or the filter’s appearance.
Overall, these results point to the need for additional research given that the low rates of adoption of chlorination diverge from results found in other contexts. Furthermore, a more intense negative emotions and social pressure messaging approach in a more well-connected community may be more effective compared to the highly mobile population in this context. Finally, the sudden decrease in soap availability after the trial ended points to open questions around behavioral barriers and coordination in providing public goods.
Dadonaite, Bernadeta, Hannah Ritchie, and Max Roser. 2018. “Diarrheal Diseases.” Our World in Data. Accessed March 29, 2023. https://ourworldindata.org/diarrheal-diseases.
Dadonaite, Bernadeta, Hannah Ritchie, and Max Roser. 2018. “Diarrheal Diseases.” Our World in Data. Accessed March 29, 2023. https://ourworldindata.org/diarrheal-diseases.