The limited impact of US workplace wellness programs on health and employment-related outcomes

Summary
In 2018, more than 80 percent of large firms and half of small employers in the United States offered a wellness program to their employees. The US workplace wellness industry’s revenue has tripled in size since 2010 to $8 billion. This growth has been partly bolstered by policies such as the Patient Protection and Affordable Care Act that encouraged firms to adopt wellness programs. Although the specific components vary widely, workplace wellness programs often include a biometric screening, health risk assessment, and promotion of wellness activities such as smoking cessation and physical activity. These programs aim to foster healthy behaviors, reduce medical spending, increase productivity at work, and improve well-being.
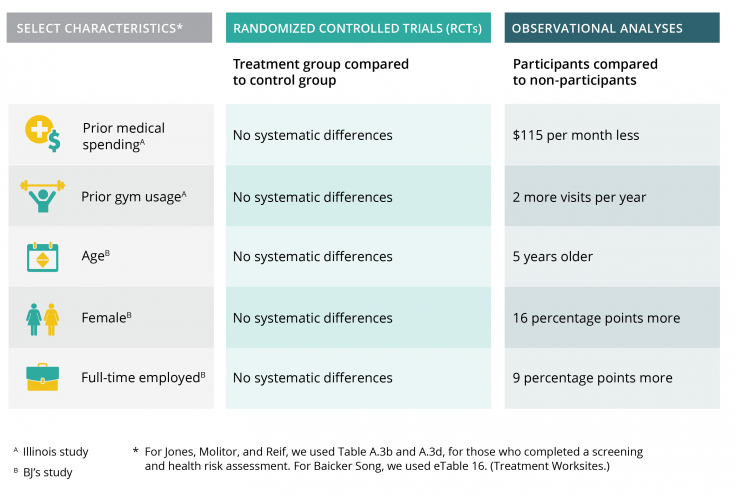
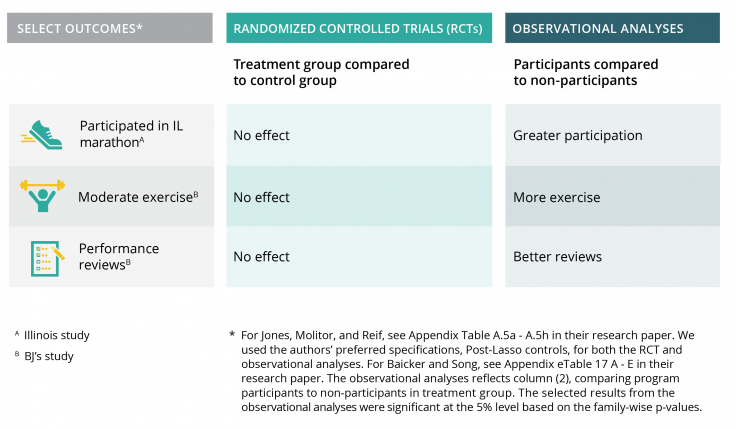
Randomized evaluations of two recent workplace wellness programs in the United States aimed to assess their impact on health and economic outcomes. These studies found that although wellness programs improved a small subset of health behaviors—such as self-reported regular exercise and weight management—they had no discernable impact on health, health care spending and utilization, or employment outcomes like absenteeism or productivity. Prior observational studies, which compared employees who participated in such programs to those who did not participate, found substantial positive associations between wellness program participation and employee health. Workers who voluntarily participate in wellness programs tend to have better health and employment outcomes regardless of whether they participate in a wellness program. Thus, these two randomized evaluations demonstrated that simply comparing participating employees to non-participants would have overstated the effect of workplace wellness programs on key outcomes.
Workplace wellness programs may have had limited impacts in part because the employees who stood to benefit the most from workplace wellness programs, such as those with poor health habits, were less likely to participate. By better targeting wellness programs, employers could potentially improve participation rates among the types of employees who are most likely to benefit from workplace wellness programs.
Supporting evidence
While two workplace wellness programs in the US improved some health behaviors, the programs had no impact on health outcomes, health care spending and utilization, and employment outcomes. Although workplace wellness programs vary widely, both studies evaluated comprehensive wellness programs that share common features with most wellness programs in the U.S. today (see Table 1) [1][2]. A key difference between the two programs was that randomization into the BJ’s Wholesale Club wellness program (BJ’s program), with worksites located across the eastern US, was at the worksite level [1]; whereas randomization into the University of Illinois at Urbana-Champaign program (Illinois program) was at the individual level [2]. After more than two years, the Illinois program improved health screening rates (a roughly 3 percentage points increase compared to about 10 percent), but had no measurable impact on other employee health behaviors, self-reported health status, medical expenditures or utilization, or employment outcomes [2]. After 18 months, employees offered the BJ’s program reported exercising more regularly (about 8 percentage points more compared to about 62 percent) and managing their weight more actively (about 14 percentage points more compared to about 55 percent) [1]. However, employees offered the BJ’s program did not have other improved health behaviors, better health, better employment outcomes, or lower health care spending [1]. Offering the program at the worksite level may have better facilitated changes in workplace culture and behavior, which could explain why the BJ’s program improved some healthy habits[1].
| BJ's Wholesale Club wellness program | University of Illinois at Urbana-Champaign program | |
|---|---|---|
| Program components | Clinical biometics Health survey 8 modules (focused on nutrition, physical activity, stress reduction), implemented by registered dietitians, each lasting 4-8 weeks | Clinical biometics Health risk assessment Wellness activities in fall and in spring (ex: smoking cessation, stress management, recreational classes) |
| Implementing organization | An established wellness provider, Wellness Workdays | The Wellness Center at the University of Illinois at Urbana-Champaign |
| Level of implementation | Worksite level | Individual level |
| Program take-up | 35% | 56% |
| Participants (compared to non-participants) | Female, nonwhite, and full-time salaried workers | Lower pre-existing medical spending and healthier behaviors |
| Length of follow-up | 18 months [36 months forthcoming] | 12 months and 24-30 months |
One reason that workplace wellness programs did not improve most measured outcomes may be because participants in wellness programs differed systematically from non-participants. Employers do not typically mandate employees to participate in wellness programs, and many employees choose not to join. In both studies, between 35 percent (BJ’s program) and 56 percent (Illinois program) of eligible employees participated in any portion of the wellness programs [1] [2]. People who chose to participate were inherently different than those who did not in ways that could predict future health outcomes [1] [2]. For example, in the Illinois study, participants had spent less on medical care the year prior and demonstrated healthier behaviors, such as more frequent gym visits and more prior running experience, compared to non-participants [2].
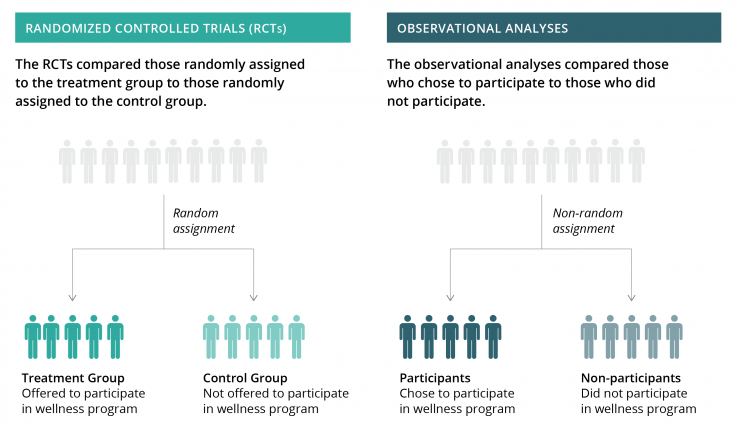
Figure 1. Comparing the randomized evaluations to observational analyses
Better targeting wellness programs might improve participation rates among employees who could benefit the most, such as employees with previously poor health habits. For example, in the Illinois program, larger financial incentives to participate in health screenings increased overall program take-up and led to more similar participation rates among different types of employees [3]. However, while larger incentives to participate in wellness activities—a different program feature—increased overall program take-up, they also increased the difference in participation between employees with previously healthy behaviors and those with less healthy behaviors [3]. More research is needed to test how to best target wellness programs to the individuals who may benefit the most from them [2].
Abdul Latif Jameel Poverty Action Lab (J-PAL). 2019. "The limited impact of US workplace wellness programs on health and employment-related outcomes." J-PAL Policy Insights. Last modified September 2019. https://doi.org/10.31485/pi.2665.2019
Song, Zirui, and Katherine Baicker. 2019. “Effect of a Workplace Wellness Program on Employee Health and Economic Outcomes.” The Journal of the American Medical Association 321 (15): 1491-1501. Research Paper | J-PAL Evaluation Summary
Jones, Damon, David Molitor, and Julian Reif. 2019. “What Do Workplace Wellness Programs Do? Evidence from the Illinois Workplace Wellness Study.” Quarterly Journal of Economics (forthcoming). Research Paper | J-PAL Evaluation Summary
Jones, Damon, David Molitor, and Julian Reif. 2019. “What Do Workplace Wellness Programs Do? Evidence from the Illinois Workplace Wellness Study.” NBER Working Paper No. 24229. Research Paper